Being told that you’re not perimenopausal because you’re still having periods
Peri-menopause is defined as the period up to 10 years before the menopause when a woman can experience menopausal-type symptoms.
Perimenopause is difficult to diagnose and is not dependent on hormone testing or your periods. You can have regular periods and normal blood hormone levels, and still be perimenopausal. This can be incredibly frustrating for women as it blocks access to appropriate treatment, and they are often left with debilitating symptoms that are inadequately treated.
A diagnosis of perimenopause is made by reviewing your symptoms and trialing different hormone treatments (hormone replacement therapy) to regulate your hormones. Feelings of anxiety, depression, irritability, fatigue and joint pain are some of the first symptoms women may experience and they are often more severe than menopause itself. Unfortunately, women are often given anti-depressants or pain medication to control their symptoms, which rarely helps.
During perimenopause, hormone levels tend to fluctuate, so your hormone levels may be controlled one day, and very high or low the next day. Perimenopause can start as early as age 30, but for many it tends to occur in the 40s. Menopause can be clinically diagnosed when a woman’s periods have been absent for a year and typically happens between the ages of 45 and 55.
The symptoms of perimenopause are often varied and far reaching. They’re similar to those of menopause, but generally exclude the changes in muscle strength and tone, reduction in bone density and vaginal atrophy.
Potential menopause symptoms:
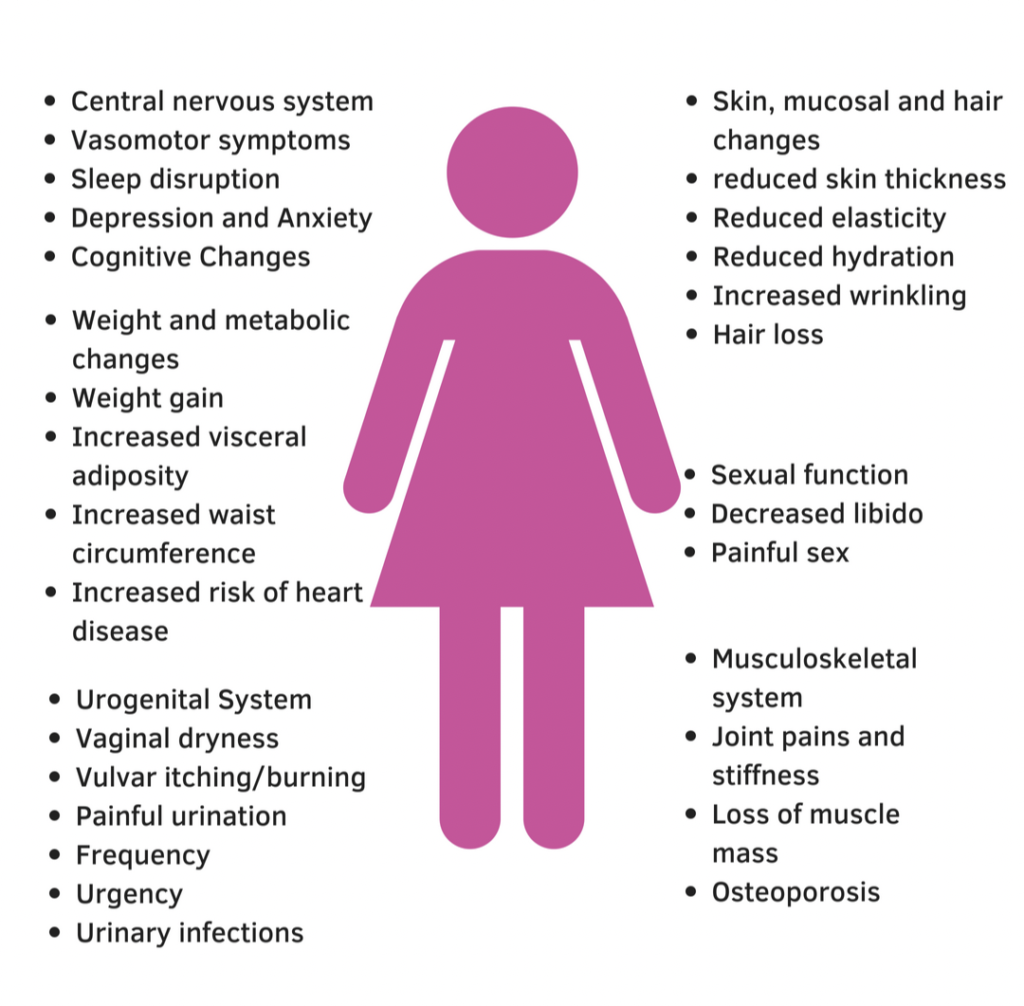 During the menopause your oestrogen levels can drop by up to 98%. Oestrogen is used in the body to strengthen bones, maintain cholesterol levels, regulate the immune system, support the heart, lubricate the vagina, help maintain body temperature and brain function and contribute to skin elasticity. Considering the pivotal role that oestrogen plays in a woman’s body it’s no wonder that a considerable drop in this hormone has a whole host of symptoms associated with it. One of the best ways of managing peri-menopause and menopause symptoms is by making lifestyle changes to help regulate your hormone levels. Eating a healthy balanced diet rich in fruit, vegetables and good quality omega 3 fats helps regulate inflammation levels in the body and counteracts some of the negative effects of oestrogen decline.
During the menopause your oestrogen levels can drop by up to 98%. Oestrogen is used in the body to strengthen bones, maintain cholesterol levels, regulate the immune system, support the heart, lubricate the vagina, help maintain body temperature and brain function and contribute to skin elasticity. Considering the pivotal role that oestrogen plays in a woman’s body it’s no wonder that a considerable drop in this hormone has a whole host of symptoms associated with it. One of the best ways of managing peri-menopause and menopause symptoms is by making lifestyle changes to help regulate your hormone levels. Eating a healthy balanced diet rich in fruit, vegetables and good quality omega 3 fats helps regulate inflammation levels in the body and counteracts some of the negative effects of oestrogen decline.
Resistance training prevents muscle atrophy (a common feature of the menopause) and assists with hormone regulation. Dynamic Reformer Pilates is one of the best ways of strengthening your body as it focuses on low-impact resistance and dynamic control. Unlike traditional weight training, reformers create natural instability, fully engaging your core and postural muscles for a whole-body workout. Pelvic and postural stability is integral to maintaining strength and function.
During the menopause and peri-menopause, we are more prone to overloading the body inadvertently, and our injury risk increases. Reformer Pilates allows you to safely progress by using springs to guide you through each movement and avoid additional strain on the joints – this should, of course, always be done under the guidance and supervision of expert and properly qualified Pilates trainers, as is provided at Ten
Continence issues during the menopause and peri-menopause are common due to pelvic floor atrophy. If you are experiencing continence issues speak to a Pelvic Health Physiotherapist to get a tailored strengthening programme. Pelvic floor strengthening under the guidance of a therapist is 70% more effective than completing pelvic floor exercises alone.
Strengthening the core, gluteal muscles and hamstrings is essential when tackling pelvic floor dysfunction but this needs to be done in a way that prevents excessive strain on the pelvic floor. Again, Dynamic Reformer Pilates is a brilliant way of targeting these muscles without overloading the pelvic floor.
Some women choose to increase their oestrogen levels with Hormone Replacement Therapy (HRT), which can greatly improve perimenopause and menopause symptoms. There has been some controversy surrounding HRT due to its link with breast cancer. However, everyone’s relative risk is different. If you are considering HRT you should speak to your GP or consult a menopause specialist.
If you’re concerned that you may be perimenopausal, or are experiencing menopause symptoms and would like to speak to one of our specialist Women’s Health Physiotherapists, please complete the following enquiry form and we’ll contact you to arrange a convenient time.
Self-paid pelvic floor consultations can also be booked online.

